Medicaid Experiments and our Multi-Trillion Dollar Food and Healthcare Revolution
Section 1115 waivers helped prove how food is indeed medicine. Now Food as Health is at work transforming our entire Food and Healthcare systems.
Note to readers: I can’t thank you enough for being here! If you like what you’re reading, please share, like, or make a comment down below. Your engagement makes all the difference in growing this newsletter.
Whether you are a healthcare or food industry stakeholder - be it a startup, community-based organization, VC, health plan, consultant, dietitian, farmer - or a consumer, the words I write here are for you.

The Rise of Food as Medicine: Beyond Disease Management
Instead of solving disease, we've built an empire around managing it. Take as directed, refill monthly, repeat indefinitely - welcome to healthcare's management merry-go-round. Our current healthcare system has been built on incentives to produce and administer therapies that manage illness. Illnesses that are so often comorbidities of metabolic dysfunction.
Food is the only tool that can reverse chronic disease stemming from insulin resistance; there is no pill that can address the root cause of metabolic ill-health. Before we developed biopharmaceutical/medical device interventions and infrastructure physicians actually prescribed specific diets that reversed disease. When insulin hit the market, patients and providers embraced medication as the de-facto therapy and dietary intervention became largely peripheral to modern medicine.
“Poor metabolic health is the primary cause of Non-Communicable Diseases (NCDs), which today make up over 74% of deaths globally.” - Swiss Re's Life and Health Spotlight: Metabolic Health, Tracking Wellbeing from the Inside Out
Enter Food as Medicine, and the narrative shifts entirely. In 2018, Blue Cross Blue Shield of North Carolina (BCBS NC) dove headfirst into the space, challenging our entire approach to healthcare delivery. By prescribing Prescriptions for Produce (ProduceRx) to address diet-related chronic disease, obesity declined (from 72% to 61%), and mental health measures increased, (from 70% to 80%). If BCBS NC were to roll out its program to its entire population, extending beyond the 555 participants who completed the trial, they estimated that medical expenses would reduce between $8.5 to $13.1 million annually.1
When positive health outcomes are associated with reduced costs and a lack of side effects, the logical next step would be widespread adoption. Yet our healthcare system continues to favor prescriptions and procedures. Why? One reason is that we're still operating in a fee-for-service (FFS) model that makes it difficult to incentivize anything that isn't billable. But there's another way: Value-based care (VBC), where the incentive shifts from services rendered to health outcomes achieved.
Take Virta Health, for example. They've proved that a well-designed ketogenic diet with proper clinical support can reverse Type 2 diabetes. They aligned their business model with patient outcomes through Value-Based Contracts, making their program free for those (e.g., employers) who hold the insurance risk for their populations, only realizing revenue when patients experience positive health outcomes. This approach could serve as a model for innovation to address the multitude of diet-related illnesses beyond Type 2 diabetes as our healthcare system shifts toward Value-based care.

From PCOS to migraines, heart disease to arthritis, there are a multitude of chronic conditions that share a common root in metabolic dysfunction (remember that root cause tree I shared last week?). We're now witnessing the early stages of a profound shift: from isolated programs to a more holistic, systematic approach. These early successes aren't just showing improved health outcomes and reduced costs - they're revealing what's possible when we shift our focus toward metabolic-disease reversal vs. management.
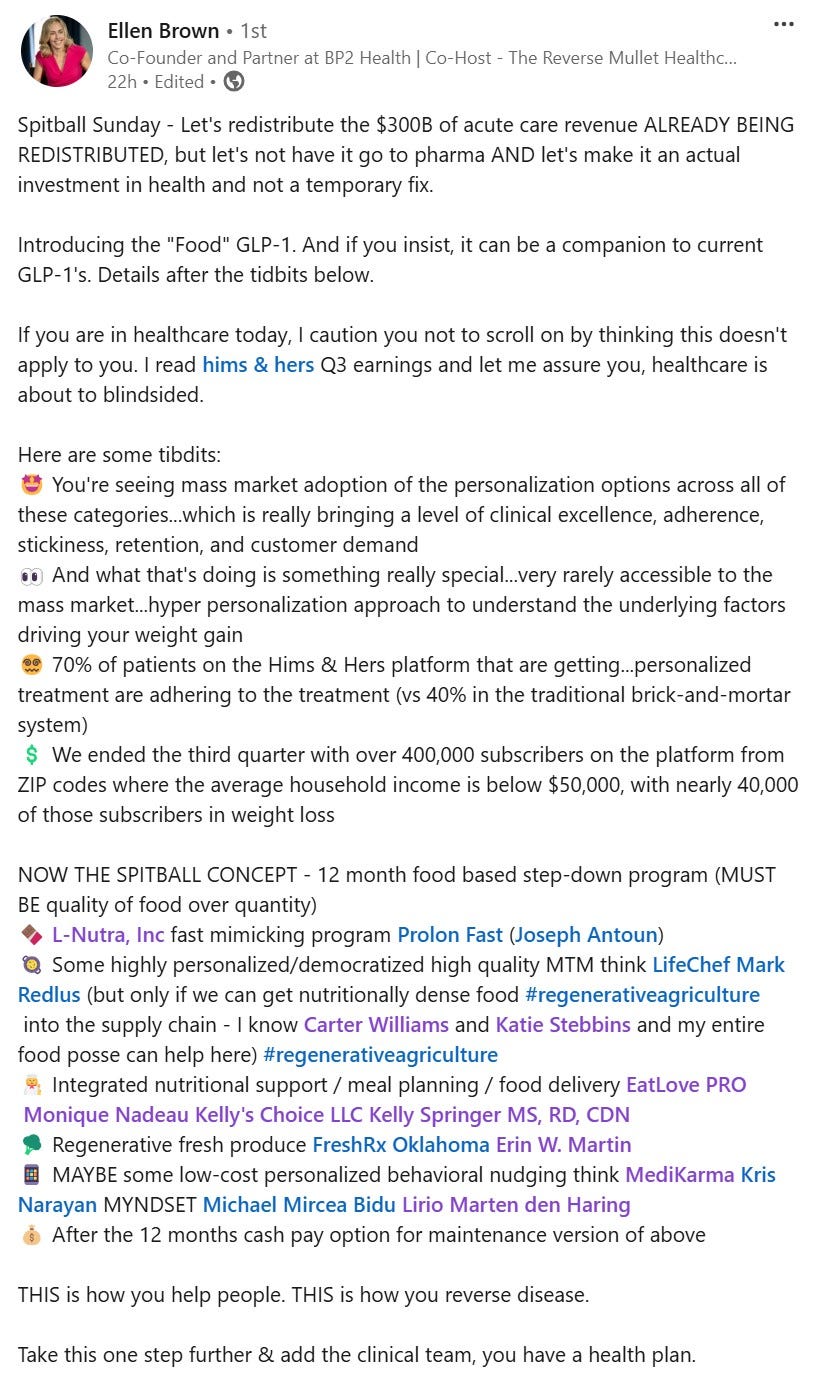
Meanwhile, the emergence of GLP-1s has done more than expose our metabolic health crisis - it's revealed how profoundly food impacts our biology. As these medications gain popularity, they're inadvertently highlighting a critical truth: both our food and healthcare systems need fundamental restructuring to support sustainable health outcomes rather than perpetual disease management.
And here's where the story gets really interesting. While Food as Medicine programs are proving what's possible on a pilot-program level, innovative healthcare and food system leaders are asking a bigger question: What if we could transform these systems entirely, making health the default rather than the exception?
Welcome to Food as Health.
Beyond Food as Medicine: Building Systems for Health
Food as Medicine programs have proved how diseases stemming from metabolic dysfunction can be reversed when patients consume more whole and less ultra-processed foods (UPFs). This revelation couldn't come at a more critical time - our healthcare system is buckling under the cost of disease management. We need solutions that can scale (*more on this later*), and we need them now.
Food as Medicine typically replaces or complements traditional medications through targeted nutrition support - think produce prescriptions or medically-tailored meals. Health plans partner with community organizations and startups to deliver these interventions, typically in the form of food delivery and/or nutrition education. Some employers offer similar programs, though they often remain stuck in the "wellness perk" category rather than being fully integrated into patient care.
The upside is clear: improved health outcomes and high patient/employee satisfaction but there are significant limitations. These programs can only reach a small segment of the population and partnerships with community-based organizations are hampered by fragmented health data infrastructures.
TECHNICAL OVERVIEW: FOOD AS MEDICINE
Current State: Replacing or complimenting medicine (e.g., GLP-1, insulin, etc.) through nutrition supports, most commonly taking the form of a Produce Prescription (where a patient receives a weekly/bi-weekly box of fresh produce) or Medically Tailored Meals.
Strengths:
Proven positive health outcomes (though there is room for improvement re. specific outcomes measured, *more to come*)
High program participant (i.e., patient/employee) satisfaction
Limitations:
Limited population reach (only certain states have nutrition supports approved for use in ‘'pilot’' programs)
Complex barriers to leveraging CBO partnerships; scaling challenges
Enter Food as Health - the broader transformation that's beginning to unfold. This approach has the ability to reach far more people by fundamentally redesigning both food and healthcare systems. While it requires significant system-level changes (accelerated, ironically, by the GLP-1 phenomenon), it offers something revolutionary: a future where we might not need Food as Medicine programs because health-promoting food and healthcare become the default.
TECHNICAL OVERVIEW: FOOD AS HEALTH
Evolution: The broader framework encompassing and expanding beyond Food as Medicine, integrating healthful foods and solutions aimed at metabolic diesease reversal more deeply within our Food and Healthcare systems.
Opportunities:
Population-wide reach
Sustained chronic disease reversal and prevention
Downstream positive externalities
Challenges:
System transformation in two well-established, highly complex industries

Food as Health transcends traditional interventions by redesigning our foundational systems - it's a fundamental shift in how we think about health creation. Instead of waiting until people are sick, our underlying infrastructures will prevent illness from happening in the first place.
🔍🔍🔍 READY FOR AN EVEN DEEPER DIVE…
Curious about how these transformations are taking place?
Subscribe to The Savory for exclusive access to:
Detailed breakdowns of Food as Medicine programs, including payment pathway evolution, implementation barriers, and success stories
Inside looks at organizations pioneering Food as Health, featuring conversations with leaders driving metabolic disease reversal at the policy, systems, and clinical levels
Future State: When Food and Healthcare Converge
Imagine a healthcare system where prevention generates more revenue than treatment, where providers prescribe food interventions as confidently as pharmaceuticals, and where continuous health creation replaces episodic disease management. Forward-thinking individuals and organizations are already proving this model works, implementing ‘Food as Medicine’ programs that bypass the current payment pathways, extending their solutions beyond pilot program cohorts and food insecurity prerequisites.
Meanwhile, our food system is transforming from the soil up. We're moving toward a future where farmers are rewarded for nutrient density over yield, and manufacturers compete on health outcomes rather than just cost.
The Bottom Line: A New Healthcare Economy
The transformation of our food and healthcare systems is underway. Organizations are proving that disease reversal is more valuable than symptom management, and the word is out on UPF’s, sugar, and the role our current nutrition guidelines play in our chronic disease epidemic. This shift is redefining how our food and healthcare systems function at their core.
And as always, I’ll leave you with a recipe.
*Recipe: Dirty, Delicious Bolognese
Note from Chérie: This is a riff on last week’s ragu bianco. You can follow the same method and I’ve highlighted (in bold italics) the addition of red vs. white wine, along with the can of tomatoes. This dish is incredible over risotto. If you’re incorporating more protein in your diet, consider adding a scoop of sauce directly into the risotto before topping with additional sauce.
Cooking time: 30 minutes prep, 30 minutes active, 3-4 hours inactive
Serves 10 - 16 as an entree, depending on how much sauce is used
Ingredients:
3 pounds of a combination of ground beef, lamb, and/or pork
1 large carrot, diced
1 onion, diced
2 celery stalks, diced
1-2 garlic cloves, minced or grated on a microplane
1-2 cups of red wine
2 cups of full-fat milk
1 large can of stewed, whole tomatoes
1 quart of chicken stock
4-6 teaspoons of salt
3-4 tablespoons olive oil or reserved fat
Method:
Heat a large pot or cast iron over medium-low heat with a few tablespoons of olive oil or reserve fat. Once warm, add carrot, celery, onion, and a few pinches of salt and let cook until they’re soft and fragrant, about 10-14 minutes. Add the garlic, stir, and let cook for 1-2 minutes more.
Using your stirring spoon, push the vegetables towards the parameter of the pan so that you can see the bottom of the pan. Add your ground meat so that it comes into contact with the pan’s surface, allowing it to develop a bit of brown crust. Eventually, you will incorporate the vegetables into the ground meat, at which point, you can add the red wine, scraping any of the tasty brown bits that have stuck to the bottom of the pot.
Once most of the wine has evaporated, add the milk and let simmer until most of the milk has evaporated, roughly 30-45 minutes.
From there, add the can of tomatoes along with the chicken stock and let cook over a gentle simmer, for roughly 4 hours for the best result.
In good health,
Chérie
P.S. - Stay tuned for a deeper dive into the individuals and organizations leading Food as Health next week!
THANK YOU FOR READING! THE SAVORY WOULDN’T BE HERE IF IT WEREN’T FOR YOUR SUPPORT ♥️
If you like what you’ve read, consider upgrading to a paid subscription, or even better, share The Savory with anyone and everyone you know!
Footnotes:




